Vaccine Urgency Increases With Extension of First Wave

The United States is still fighting the first wave of the coronavirus pandemic—not the dreaded “second wave.”
“When you have 20,000-plus infections per day, how can you talk about a second wave?” says Dr. Anthony Fauci of the National Institutes of Health. “We’re in the first wave.”
Echoing that perspective, Dr. Arnold Monto, a University of Michigan flu expert, characterized the current state of the pandemic as “continued transmission with flare-ups.”
The good doctors were making the point that a graph of infectious disease cases resembles the peaks and troughs of a wave in the ocean.
In the United States, the number of new coronavirus cases declined somewhat at the start of summer, but daily totals never approached zero. Far from it.
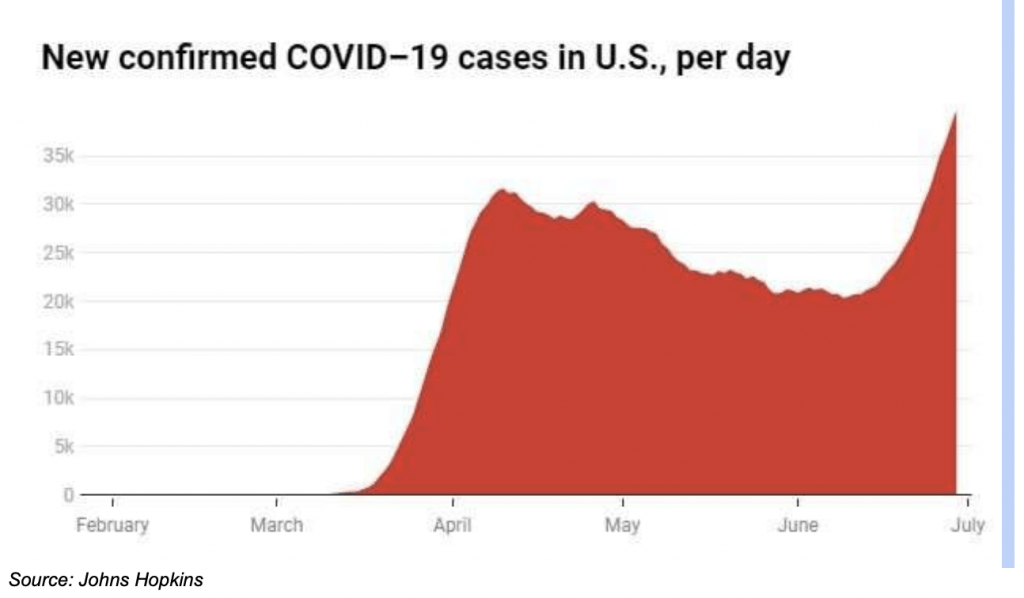
The first wave of the coronavirus is still rolling, leaving destruction in its wake. And no one can accurately predict when the first wave might end.
Meanwhile, on July 3, the United States set the world record for the most new infections per day at around 55,000. It’s all but guaranteed that even more cases were recorded over the July 4 holiday as massive crowds of Americans ignored public health guidelines.
In the heat of the first wave, a question remains unanswered: What would constitute the transition from the first wave to the second?
The disease would have to be strictly controlled, with transmission rates reduced to a very low level, for the first wave to be considered “contained,” epidemiologists say. That would amount to hundreds of new infections per day, not tens of thousands.
After reaching that point, a second wave would theoretically begin if the number of new infections per day climbed back into the thousands, alongside a resurgence in hospitalizations.
If the first wave somehow ends this summer, most experts fear a second wave would materialize in the fall as people retreat indoors because of falling temperatures. Research indicates transmission rates will be higher in fall and winter because indoor transmission is much more likely than outdoor.
So a second wave would likely coincide with the “normal” flu season, adding to the burden of an already-strained public health system.
Also, the coronavirus is probably mutating, making it even harder to contain. In fact, a mutation already in progress (COVID-19 2.0) could be even more contagious than the original, researchers suggest in a study published July 3 in the periodical Cell.
Research in China confirms that possibility. Authorities there have adjusted their official quarantine guidelines from 14 days to 28 days because they believe a more durable mutated version of the may already be circulating.
It’s enough to push the collective consciousness into a bottomless pit of despair—except that important developments in testing, treatment and vaccination are countering the negative tide and providing hope.
A new COVID-19 “paper strip” test is showing early promise. It’s licensed by the Wyss Institute of Harvard and was developed in conjunction with privately held Sherlock Biosciences. The test, intended for self-administration at home, appears safe, simple and relatively inexpensive, representing a big step forward in identifying and possibly containing the virus.
A new drug treatment for the coronavirus is likewise producing promising results. The drug, known as dexamethasone, is a type of steroid—a group of drugs that has traditionally been prescribed for treating inflammation.
In severe cases, COVID-19 can trigger an out-of-control immune response, which often results in extreme inflammation. Dexamethasone provides assistance in tempering the body’s immune response. India-based Cadila Healthcarehas emerged as one of the biggest producers of the drug.
Dexamethasone has previously been used to treat rheumatoid arthritis, an affliction often associated with a dysfunctional immune response. Treatment for rheumatoid arthritis may hold crossover potential for COVID-19 because dysfunctional immune responses tend to be common problems in both disorders, as Luckbox previously reported.
One final glimmer of hope is appearing on the vaccine front. Vaccines are usually the most effective method of containing (and ending) pandemics because they provide immunization to healthy people.
Last week, researchers from a well-publicized vaccine development project at Oxford University released data suggesting that patients inoculated with their experimental vaccine had exhibited a strong antibody response—even stronger than the antibody buildup in so-called “recovered” coronavirus patients.
That suggests the Oxford vaccine candidate could provide sustained immunization from COVID-19, as opposed to only temporary protection. The vaccine being developed at Oxford, in conjunction with AstraZeneca (AZN), is currently in Phase II trials.
Readers who want to follow developments related to the pandemic, or anything else that’s moving the financial markets, can tune into TASTYTRADE LIVE weekdays from 7:00 a.m. to 3:00 p.m. Central time.
“Sage Anderson” is a pseudonym for a contributor who has traded equity derivatives and managed volatility-based portfolios as a prop trading firm employee. He is not an employee of Luckbox, tastytrade or any affiliated company. Readers may direct questions about this blog post or any other trading-related subject, to support@luckboxmagazine.com.